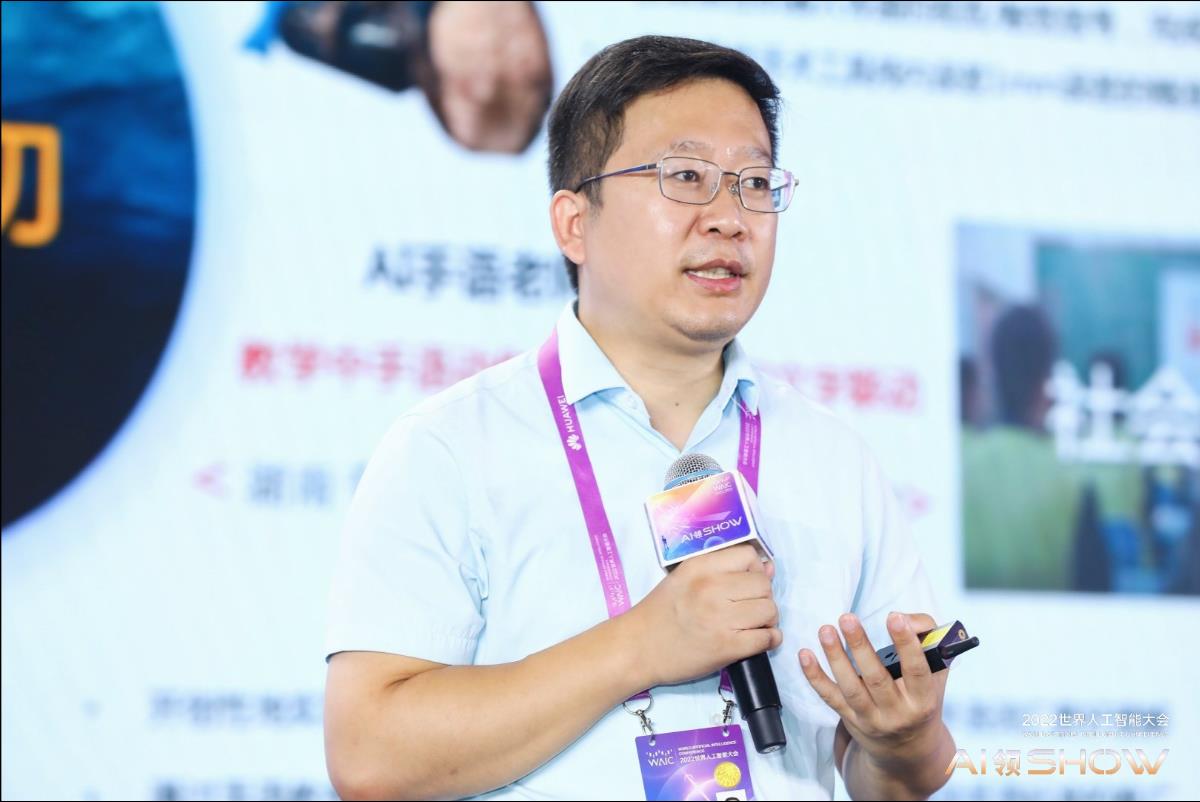
About the author:Li Baowei, Wu Wei, Department of Otolaryngology, 306th Hospital of PLA.
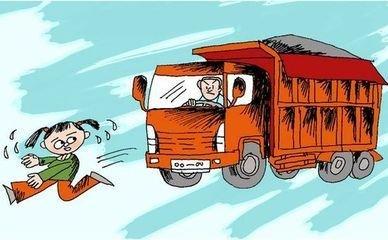
March 21st is the 16th World Sleep Day sponsored by the International Mental Health Organization. The China Sleep Research Association held a press conference recently, saying that 80% of major traffic accidents are related to drivers’ lack of sleep. Driving without sleep for 17 hours in a row, the risk of accidents is "equivalent to drunk driving". The seminar also specifically reminded that drivers with "sleep apnea syndrome" are potential road killers. People with this sleep disorder repeatedly experience apnea during sleep, and hypoxia affects organ function, resulting in poor sleep quality, daytime sleepiness and slow response.
On the occasion of "World Sleep Day", the author makes a brief introduction to the basic knowledge of "Sleep Apnea Syndrome", which seriously affects people’s health and safety.
The scientific name of Sleep Apnea Syndrome is Obstructive Sleep Apnea Hypopnea Syndrome (OSAHS), commonly known as "Snoring", which is mainly caused by the relaxation of muscles that keep the upper airway open during sleep, and the airway collapses and blocks, resulting in a sleep-disordered disease characterized by snoring and apnea. Its main harm lies in the frequent occurrence of sleep apnea and hypoventilation, which leads to the intermittent decrease of oxygen saturation, which leads to a series of pathological changes in human body and becomes the source disease of many systemic diseases (diabetes, hypertension, coronary heart disease, cerebrovascular accident, etc.). People who suffer from snoring are prone to drowsiness, inattention, memory loss, low work efficiency, easy to make mistakes when engaged in high-risk industries, and especially prone to traffic accidents when driving. Many serious traffic accidents are related to fatigue driving and illegal driving, and a considerable part of fatigue driving is related to drivers suffering from OSAHS. According to the survey, more than 50% drivers who snore suffer from hypoxia (hypoxemia) during sleep, which easily leads to dozing off while driving during the day and greatly increases the probability of traffic accidents.
1. What are the causes of OSAHS?
The cause of OSAHS is the stenosis and obstruction of the upper airway, but it is not a simple airway obstruction, but actually the collapse of the upper airway, accompanied by the disorder of respiratory central nervous regulation factors. There are many reasons for upper airway stenosis and obstruction, including nasal septum curvature, tonsil hypertrophy’s disease, long soft palate, mandibular arch stenosis, mandibular retraction deformity, temporomandibular joint ankylosis, micrognathia secondary to bilateral joint ankylosis, giant tongue disease, hyoid bone retroversion, etc., obesity, mucous edema of upper airway tissue, and oropharyngeal or hypopharyngeal tumors can also cause OSAHS. Some endocrine diseases can also be combined with this disease. Its pathogenesis may be related to the increase of soft tissue and muscle collapse in upper airway during sleep, and the decrease of stimulation reactivity of upper airway muscles to hypoxia and carbon dioxide during sleep. In addition, it is also related to the comprehensive effects of nerves, body fluids, endocrine and other factors.
Second, what are the manifestations of OSAHS?
(1) Performance during the day

1. Sleepiness: The most common symptom is drowsiness and lethargy during daytime work or study. In severe cases, you can fall asleep while eating or talking with people, and even have serious consequences, such as falling asleep while driving and causing traffic accidents.
2, dizziness and fatigue: due to repeated apnea and hypoxemia at night, the continuity of sleep is interrupted, the number of awakenings increases, the quality of sleep declines, and there are often slightly different dizziness, fatigue and fatigue.
3. Abnormal mental behavior: inattention, decreased fine operation ability, decreased memory and judgment, inability to do work when symptoms are serious, and senile people may show dementia. The brain damage caused by hypoxemia at night and the change of sleep structure, especially the decrease of phase during deep sleep, are the main reasons.
4. Headache: It often appears in the early morning or at night, and the dull pain is common, not severe, lasting for 1-2 hours, and sometimes it needs to be relieved by taking painkillers, which is related to the increase of blood pressure, intracranial pressure and changes in cerebral blood flow.
5, personality changes: irritability, excitability, anxiety, etc., family and social life are affected to some extent, due to the gradual alienation from family members and friends, depression may occur.
6, sexual dysfunction: about 10% of patients can have decreased libido and even impotence.
(2) Performance at night
1. Snoring: it is the main symptom. Snoring is irregular and varies in height. Snoring-air flow stops-panting-snoring often appears alternately. Generally, the air flow is interrupted for 20-30 seconds, and some cases last for more than 2 minutes. At this time, patients may have obvious cyanosis.
2. Apnea: 75% of the people who sleep in the same room or bed find that the patient has apnea, and they often worry that the breathing will not recover and push the patient to wake up. Apnea usually ends with panting, holding back or loud snoring. Patients with OSAHS have obvious contradictory breathing between chest and abdomen.
3, waking up: suddenly waking up after apnea, often accompanied by turning over, involuntary movement of limbs or even convulsions, or suddenly starting, feeling flustered, chest tightness or discomfort in the precordial area.
4, restless: due to hypoxemia, patients turn over and rotate more frequently at night.
5, hyperhidrosis: sweating more, especially in the neck and upper chest, related to hypercapnia caused by respiratory force and apnea after airway obstruction.
6. Nocturnal urine: Some patients complained that the number of urination at night increased, and some cases had enuresis.
7. Abnormal sleep behavior: manifested as fear, screaming, delirium, night walking, auditory hallucination, etc.
(3) Manifestations of systemic organ damage

Patients with OSAHS often take abnormal cardiovascular system as the first symptom and sign, which can be an independent risk factor for hypertension and coronary heart disease.
1. Hypertension: The incidence of hypertension in OSAHS patients is 45%, and the therapeutic effect of antihypertensive drugs is not good.
2. Coronary heart disease: manifested as various types of arrhythmia, nocturnal angina pectoris and myocardial infarction. The twentieth is due to the damage of coronary artery endothelium caused by hypoxia, the deposition of lipids in the intima of blood vessels, and the increase of erythrocyte and blood viscosity.
3. Various types of arrhythmia.
4. Pulmonary heart disease and respiratory failure.
5, ischemic or hemorrhagic cerebrovascular disease.
6, mental disorders: such as manic psychosis or depression.
7. Diabetes.
Third, how to determine whether you have OSAHS?
According to the patient’s snoring with apnea, daytime sleepiness, obesity, thick neck circumference and other clinical symptoms, a preliminary clinical diagnosis can be made, and the severity and type of the disease can be confirmed and understood, so corresponding examinations are needed. Polysomnography (PSG) monitoring is the gold standard for the diagnosis of OSAHS, and can determine its type and severity. Routine ear, nose, throat and oral examination were performed on the diagnosed OSAHS to find out whether there were any local anatomical and developmental abnormalities, hyperplasia and tumors. X-ray photos of skull and neck, CT and MRI are used to measure the cross-sectional area of oropharynx, which can be used to judge the location of stenosis. Some patients can be tested for endocrine system.
Fourth, how to treat OSAHS?
1. General treatment: (1) Weight loss: diet control, drugs and surgery; (2) Sleep posture change: sleep sideways and raise the bedside; (3) Quit smoking and drinking, and avoid taking sedatives.
2. Drug treatment: There is no specific drug at present, and the curative effect is uncertain. Modafenib can improve daytime sleepiness, and it has a certain effect on patients whose sleepiness symptoms are not obviously improved after CPAP treatment.
3. Instrument therapy: (1) Nasal-continuous positive airway pressure (CPAP). Indications include AHI≥15 times/hour; AHI<15 times/hour, but daytime sleepiness and other symptoms are obvious; Patients with surgical treatment failure or recurrence; Can’t tolerate other treatment methods. Contraindications include coma, pulmonary bullae, hemoptysis, pneumothorax and unstable blood pressure. (2) Bi-level positive airway pressure (BIPAP) therapy. (3) Auto-CPAP ventilator therapy. (4) oral appliance (OA) therapy. The indication is simple snoring; Patients with mild and moderate OSAHS; Can’t tolerate other treatment methods. This method is not suitable for people with temporomandibular arthritis or dysfunction.
4, surgical treatment: (1) nasal surgery; (2) Palatoplasty; (3) laser-assisted pharyngoplasty; (4) radiofrequency ablation at low temperature; (5) Orthognathic surgery.
5. How to prevent OSAHS?
1. Strengthen physical exercise and maintain good living habits.
2. Avoid alcohol and tobacco hobbies, because smoking can aggravate respiratory symptoms, and drinking can aggravate snoring, nocturnal respiratory disorders and hypoxemia. Especially drinking before going to bed.
3. For obese people, we should actively lose weight and strengthen exercise. Our experience is to lose more than 5%~10% of weight.
4. Snoring patients often have decreased blood oxygen content, so they are often accompanied by high blood pressure, arrhythmia, increased blood viscosity and increased heart burden, which may easily lead to cardiovascular and cerebrovascular diseases. Therefore, it is necessary to pay attention to blood pressure monitoring and take antihypertensive substances on time.
5, it is forbidden to take sedatives and sleeping things before going to bed, so as not to aggravate the inhibition of respiratory center regulation.
6. Take a lateral sleeping position, especially the right lateral sleeping position, to avoid the tongue, soft palate and uvula falling after relaxation during sleep, which will aggravate the upper airway obstruction. You can wear a small ball on your back during sleep, which is helpful to keep sleeping on your side.